Troubleshooting an Electromyograph Twitch Monitor
It’s easy to figure out why your monitor isn’t working, just follow these steps
All patient monitors require troubleshooting from time to time. It’s good to have a methodical approach and it’s not difficult. This guide can be used for any electromyograph monitor, but we use the example of the TwitchView, which is the monitor we use in our hospitals.
1. Place the electrode array over the ULNAR nerve
If you are not getting the result you expect either because there is NO EMG WAVEFORM or the EMG WAVEFORM IS VERY SMALL, the first thing to do is make sure the stimulating electrodes are properly placed over the ULNAR nerve, which is on the little finger side of the forearm, not in the middle of the forearm and not on the thumb side of the forearm. The ulnar nerve is closer to the edge of the forearm than most people think—see Figure 1. It is very easy to become confused and put the stimulating electrodes on the thumb side of the forearm. Even very experienced users do this from time to time. This will not give a good result.
Figure 1. Location of the ulnar nerve at the wrist is marked by green circle as the site of stimulating electrodes placement. When the wrist is fully extended, one can often see a depression in the skin indicating the location of ulnar nerve.
2. Make sure the electrode array is connected properly to the cable.
It is difficult but possible to put the connect into the cable upside down. Check to be sure it is right side up as shown in Figure 2. Be sure the connector on the electrode array slides all the way into the connector on the cable.
Figure 2. Panel A shows electrode array connector plugged into the cable upside down and not fully inserted. Panel B shows correct orientation of the electrode array connector and cable plug with electrode array connector fully inserted into cable plug.
3. Turn up the current
When the TwitchView is started, it will automatically determine the “supramaximal current” that is required to depolarize the ulnar nerve. This current will often be less than the maximum output, which is 80mA. Under some circumstances, the supramaximal current can change during the course of a case. For example, repositioning the arm can alter the relationship between the stimulating electrodes and ulnar nerve. When in doubt, TURN THE CURRENT UP TO 80mA. We do not know of any risk of harm from doing this, at least in adult sized patients (there is remarkably little known about twitch monitoring in small children and babies—we will have a guest post from a pediatric twitch monitoring expert in the future). We always operate TwitchView (or any other similar monitor) at 80mA (or the maximum available—some monitors’ maximum is <80mA)[*]. It is all benefit and no risk. You might ask if we recommend operating at 80mA, why does anyone bother with determining the supramaximal current. Indeed, it is unwise to operate BELOW the supramaximal current (which is a reason to measure it), which may result in poor ulnar nerve stimulation, but there is no penalty for operating ABOVE the supramaximal current.
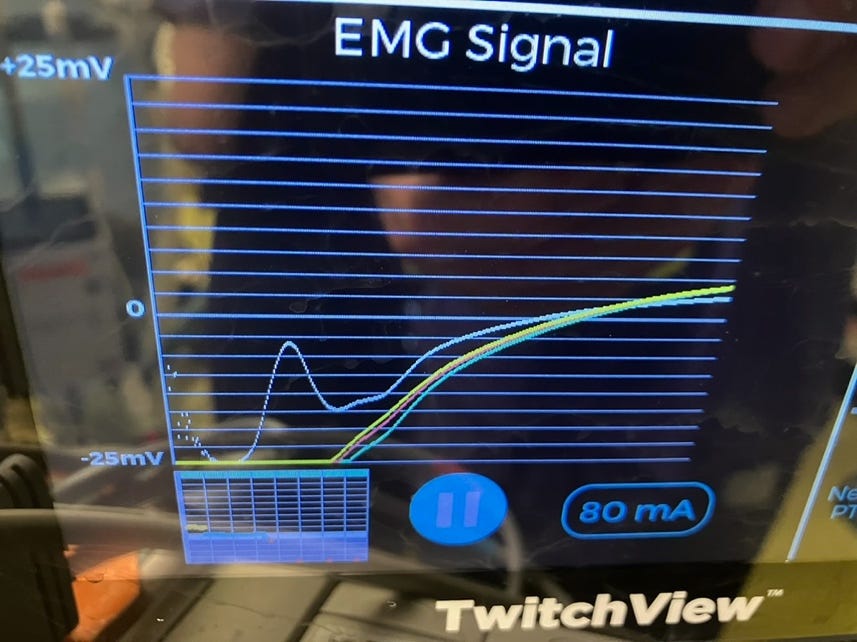
4. Replace the cable
After confirming that the electrode array is in the proper location, if you still have no EMG waveform (and you are positive that the patient is not entirely paralyzed!), or a bizarrely shaped waveform that makes no sense at all (example shown in Figure 3), change out the cable. Cables for all types of monitors get beat up very badly in their daily life in the OR and failure is not uncommon due to fractures of conductors, wear and tear on connectors, fluids in the cable-end receptacle etc. In our experience, cables are much more likely to be at fault than single-use sensors (such EMG electrode arrays, BIS sensors, pulse oximeters, pressure transducers). We usually will change the cable before replacing a sensor, unless the sensor is obviously damaged. We are just playing the odds. If we still don’t have a working monitor after replacing the cable, we will replace the sensor, but bad sensors are rare. It is also very rare to have the monitor “box” fail, although it is not impossible.
Figure 3. A bizarre EMG waveform that could be caused by a bad cable.
5. The electrode array may be loose
It is possible for the electrode array to be loose and either fail to produce a proper EMG waveform and NOT trigger the automatic electrode impedance warning in the machine. Signs of a loose electrode include bizarrely shaped EMG waveforms (also may occur with a bad cable) or twitch responses that jump around. Normally during recovery from neuromuscular blockade there is a smooth progression. If the train-of-four count or ratio jumps around a lot as in Figure 4, the electrode might be loose. If the arm being monitored is accessible, it’s easy to check. If the arm is tucked, then wait until the end of the case, inspect for a loose electrode and refasten if needed. Remember that if there is a monitoring failure during a case with the arm tucked, it’s always possible to troubleshoot and check the twitch response when the arm is accessible at the end of the case. Always make sure the patient is adequately recovered or reversed.
Figure 4. In the upper 2 frames are normal TwitchView trend plots. Note how smooth the data are with virtually no scatter from point to point. In the lowest frame is a trend plot from a loose electrode showing marked scatter between data points.
6. Change the sensing electrode
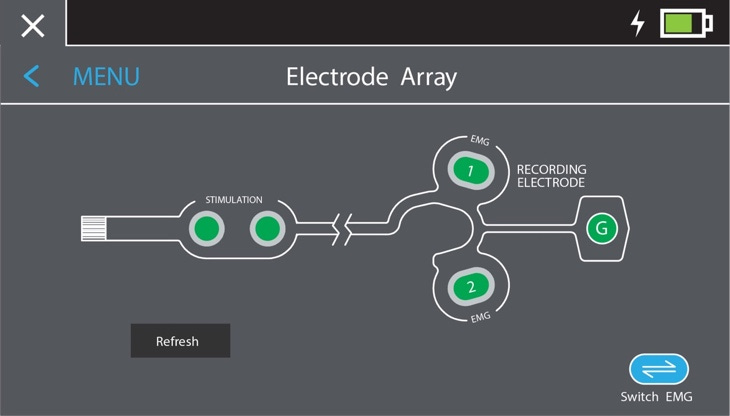
The TwitchView monitor has 2 sensing electrodes on opposite sides of the thumb, but only uses one at a time. When determining the supramaximal current the monitor will choose the electrode with the best signal. However, you can override this and select the other sensor (see Figure 5). If you are having problems with signal quality, this can be worth a try.
Figure 5. Screen shot of TwitchView electrode array menu for switching between sensing (recording) electrodes 1 and 2.
General points—
1. It is wise to start the monitor after the patient is asleep but prior to administering a neuromuscular blocking drug. If the monitor isn’t delivering a proper EMG waveform, you know for sure it’s not because the patient is paralyzed, and troubleshooting becomes more transparent.
2. If you have given neuromuscular blocking drugs, always consider the possibility that the patient is paralyzed if there is no twitch. We have seen many cases where providers were sure the monitor was not working, but in fact their patient was paralyzed. Rocuronium has a very wide range of clearance from patient to patient, and in some patients the duration of action far exceeds what people tend to expect.
[*] We always conduct our research studies of twitch monitors at 60mA, because we do some comparative studies in which 60mA is the maximum current output of one or more of the monitors